Wisdom teeth, also called third molars, are the last teeth that grow in the mouth and they usually appear between the ages of 16 to 25.
These teeth can only properly grow if they have enough space in the back of the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not happen all the time.

The extraction of wisdom teeth is necessary when they are prevented from properly erupting into the mouth. They may grow sideways, partially emerge in the mouth, and even remain trapped beneath the gum within the jaw. These impacted teeth can eventually cause severe infections, cavities and move other teeth.
The most serious complications occur when tumors or cysts form around the impacted wisdom teeth, resulting in the destruction of the jawbone and healthy adjacent teeth. The early removal of the third molar tooth usually avoids these problems and decreases surgical risks involved with the procedure.
Not all wisdom teeth cause issues, but many do. Removal may be recommended if you experience:
A detailed exam and imaging help determine whether your wisdom teeth should be removed now or monitored over time.
Pericoronitis (infection/inflammation around partially erupted tooth)
Caries (decay) in the wisdom tooth or adjacent 2nd molar
Periodontal pathology / bone loss around 2nd molar
Cyst or benign tumor (dentigerous cyst, odontogenic keratocyst)
Root resorption of adjacent 2nd molar
Any significant pathology requiring removal (combined)
1–5% (higher if partially erupted)
1–4% per year
0.5–2% per year (detectable progression)
0.01–0.1% per year (≈1 in 1,000 to 1 in 10,000 per year)
<0.1% per year
≈1–6% per year (age-dependent)
Highest risk in 20–29-year-olds; ~25% lifetime risk if partially erupted
Increases with age and partial eruption
Long-term studies show ~25–50% of retained asymptomatic teeth develop periodontal defects over 10–20 years
Very rare; most cysts found incidentally on radiographs; lifetime risk ≈2–4% for fully impacted teeth
Rare but serious when it occurs
Highest in early 20s (up to 5–6%), drops significantly after age 40
Even when wisdom teeth don't cause pain, they can pose ongoing health risks. Research shows that keeping impacted teeth requires vigilance, as complications can develop silently over time.
The most frequent complications involve infection and tooth decay.
Pericoronitis (inflammation of the gum tissue) affects approximately 1–5% of retained teeth annually, with the highest risk occurring in patients aged 20–29.
Similarly, cavities (caries) can develop in the wisdom tooth or the adjacent molar at a rate of 1–4% per year, as these areas are often difficult to clean effectively.
Periodontal health is a significant long-term concern. While annual bone loss around the second molar is gradual (0.5–2% per year), the cumulative effect is significant.
Long-term studies indicate that 25–50% of retained asymptomatic teeth will eventually develop periodontal defects over a 10 to 20-year period.
While much less common, serious pathologies can occur.
Cysts or benign tumors develop in rare cases (approximate annual risk of 0.01–0.1%), usually discovered incidentally on X-rays.
Root resorption, where the wisdom tooth damages the root of the adjacent healthy molar, occurs in less than 0.1% of cases annually but requires immediate attention when identified.
Age plays a major factor in these risks. Patients between 20 and 25 years old face the highest probability (approx. 3–6%) of developing a problem requiring removal. This risk drops to about 1–3% for patients aged 26–35.
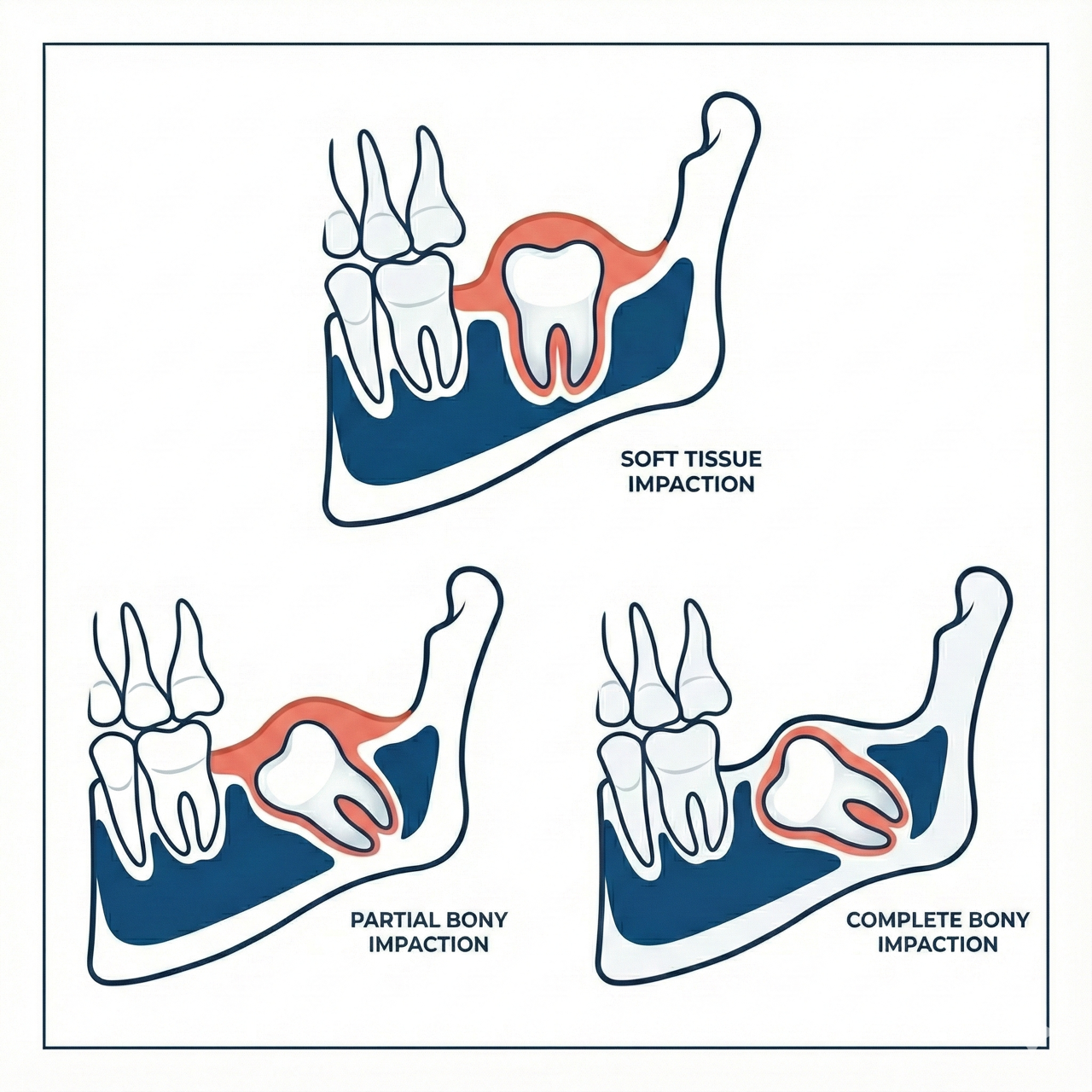
Wisdom teeth can be positioned in different ways beneath the gums:
Soft Tissue Impaction – The crown of the tooth is covered by gum tissue, making cleaning difficult and increasing the risk of infection.
Partial Bony Impaction – Part of the tooth is still within the jawbone. These teeth may cause repeated infections or decay.
Complete Bony Impaction – The entire tooth remains in the jawbone. Removal may be recommended to prevent future problems such as cysts or damage to nearby teeth.
Your surgeon will review your imaging and explain the position of your teeth and what that means for treatment.
Wisdom tooth removal is a routine procedure at our clinic. We focus on comfort, efficiency, and safety from start to finish.
During your appointment:
For anxious patients, sedation can be an excellent way to make the experience much easier.
For more information about the recommendations before and after surgery, please visit our pre-operative and post-operative pages.


Most patients recover quickly and comfortably after wisdom tooth removal.
We provide clear instructions on how to care for the area, what foods to choose, and how to minimize the risk of dry socket. If anything feels unusual during recovery, we encourage you to contact our office.
Late teens to early twenties is ideal because the roots are not fully developed and healing is generally faster.
You can choose from several sedation options but general anesthesia is useful to ensure a calm and comfortable experience.
Not always. Some can stay in place if they are healthy, fully erupted, and easy to clean. We assess each case individually.
Soft foods such as soups, smoothies, eggs, and mashed potatoes are best during the first few days.
Don't wait until discomfort sets in. Schedule your consultation today for a smooth wisdom teeth removal experience.